Cortisone... this subject has been a sore spot for me for many years. It is one that I feel passionately about as it directly opposes everything I believe and everything I know about medicine.
Corticosteroids are drugs synthesized in a laboratory that resemble cortisol, a hormone produced by the adrenal glands that temporarily reduces the immune system’s activity. Since their introduction in 1935 as a treatment for Addison’s Disease, steroids have since been used for their anti-inflammatory and immune-modulating properties. A 2014 report by Ericson-Neilson and colleagues discusses how steroids are used in clinical practice. Read more.
When inflammation stops, healing stops also.
Cortisone injections are effective in reducing pain because they temporarily reduce the inflammation causing the pain. The problem is that inflammation is the body’s method of healing. Learn more. When inflammation stops, healing also stops. Certainly, excessive inflammation is to be avoided, but long-term treatment by cortisone and NSAIDs is not the answer. Procedures that address the root cause of inflammation give better long-term results without the side effects associated with synthetic substances.
Damage caused by cortisone to joint tissue advances the symptoms of degenerative arthritis.
The ends of bones are covered by smooth articular cartilage that protects the bones in the joint. This tissue allows the bones to glide smoothly, reducing friction and subsequent inflammation. Over time, cortisone injections often deteriorate tissue, increasing friction and causing painful inflammation, resulting in further advancement of arthritic conditions.
Effects of cortisone on cartilage can include:
- Thinning of cartilage which can have a negative long-term impact on joint health.
- Loss of cartilage tissue, especially with repeated injections.
- Cortisone injections can also cause damage such as clumping of collagen, changes in cell shape, and necrosis.
Study Findings
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
Numerous studies have shown the negative effects of cortisone injections. Particularly notable are those funded by the NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). A 2017 study by McAlindon et al appearing in the Journal of the American Medical Association showed that “...repeated steroid injections over two years brought no long-term improvement in reducing pain... Rather than showing any benefit, the results revealed that the injections sped the loss of the cartilage that cushions the knee joint.”
Study conclusions: Among patients with symptomatic knee osteoarthritis, 2 years of intra-articular triamcinolone, compared with intra-articular saline, resulted in significantly greater cartilage volume loss and no significant difference in knee pain. These findings do not support this treatment for patients with symptomatic knee osteoarthritis. McAlindon T, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical trial. JAMA. 2017;16;317(19):1967-1975.
Mayo Clinic
The Mayo Clinic warns of the risks with use of corticosteroids to reduce pain of arthritis. Potential side effects of cortisone shots increase with larger doses and more frequent use. Side effects can include:
- Cartilage damage.
- Death of nearby bone.
- Joint infection.
- Nerve damage
- Short-term flare of pain, swelling and irritation in the joint.
- Short-term increase in blood sugar.
- Tendon weakening or rupture.
- Thinning of nearby bone (osteoporosis).
- Thinning of skin and soft tissue around the injection site.

Cellular Physiology
Research findings help direct physician course of treatment, but the cellular physiology of how cellular changes occur is fascinating. A comprehensive article by Ron Hauser, MD published in the May 2009 issue Journal of Prolotherapy helps explain the healing process and why damage to tissue occurs.
...corticosteroid injections into normal and degenerated knees accelerate the arthritic process. A summary of the effects of the intraarticular corticosteroids on articular cartilage includes: a decrease of protein and matrix synthesis, matrix hyaline appearance becomes fibrotic, clumping of collagen, alteration in chondrocyte cell shape, chondrocyte cell proliferation inhibited, chondrocyte cytoxicity enhanced, loss of chondrocytes, surface deterioration including edema, pitting, shredding, ulceration and erosions, inhibition of articular cartilage metabolism, articular cartilage necrosis, thinning of articular cartilage, decrease in cartilage growth and repair, formation of articular cartilage cysts, and ultimately articular cartilage destruction.
Chondrocytes
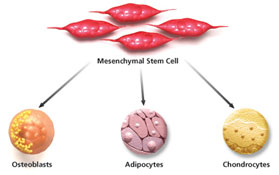
Chondrocytes are the cells responsible for the formation, maintenance, and repair of articular cartilage. They produce collagen and the extracellular matrix important in maintenance of cartilaginous tissue. They originate from bone marrow mesenchymal stem cells. Stem cells differentiate into progenitor cells that remain available in tissue to maintain homeostasis, a balance between available healing cells and requirements for tissue maintenance. The proliferative capacity is controlled by chondrocytes. The complexity of articular cartilage repair and regeneration are discussed by Rodrigo Somoza and colleagues in Tissue Engineering. Learn more.
The aim of cellular medicine is to increase the number of mesenchymal stem cells to compensate for depletion of available chondrocytes resulting from chronic degeneration or acute requirement. This influx of stem cells and other growth cells and nutrients helps to re-establish homeostasis.
Chondrocytes make up one to five percent of the volume in adult cartilage tissue. Despite a poor oxygen tension, limited nutrient supply, and anaerobic metabolism, chondrocytes can still produce large amounts of collagen and proteoglycans. The collagen provides strength to the cartilage, the proteoglycans provide elasticity and stiffness on compression. (Hauser et al. J of Prolotherapy,2009.)
Hauser further discusses the function of the cells that are affected by use of corticosteroids, particularly the function of chondrocytes.
...loss of protein polysaccharide in the matrix, decreased number of chondrocytes, loss of cell shape, distortion of the cell membrane and nucleus leading to chondrocyte degeneration, multiple fissuring of the matrix, clumping of collagen, and finally by the sixth month, appearance of large cysts containing debris and degenerated chondrocytes.
The catabolic effects of intraarticular corticosteroids include a massive decrease in the synthesis of all major articular cartilage matrix components. The loss of glycosaminoglycans, proteoglycans, proteins and matrix collagen leads to the ultimate breakdown of the articular cartilage. The net result of corticosteroid joint injections is an acceleration of the osteoarthritic process which is manifested in the dramatic rise of cases of osteoarthritis of the knee and hip and subsequent joint replacements. (Hauser et al. J of Prolotherapy,2009.)
Bone Density
Theodore R. Fields, MD, FACP, Attending Physician, Hospital for Special Surgery and Professor of Clinical Medicine, Weill Cornell Medical College, discusses how “Steroid therapy can cause thinning of the bones and increase the risk of bone fractures... a person can lose 10%-20% bone mass within the first six months of corticosteroid therapy.” Read more.
The topic of bone mass and the damaging effects of cortisone is further discussed by William Ericson-Neilsen, MD published in the Summer 2014 edition of The Ochsner Journal. NIH
Corticosteroids impair the mineralization of bone matrix by initially favoring the activity of osteoclasts (during the first 6 to 12 months of therapy) while also inhibiting the absorption of calcium in the gut. Corticosteroids have also been shown to cause a decrease in bone formation by reducing the activity and lifespan of osteoblasts, promoting their apoptosis as well as the apoptosis of osteocytes.
Steroids Destroy Stem Cells
A key component of medicine at NTXMSK is the role that mesenchymal stem cells play in healing the musculoskeletal system. Understanding of the multiple functions of stem cells and their role in tissue repair is still developing. We do know that their presence is key in stimulating the body's natural repair system by inducing the proliferation of cells. This happens several different ways:
- Localized mesenchymal stem cells (MSCs) live in tissue where they can be activated to develop (differentiate) into the type of tissue where they reside. These body (somatic) stem cells continually divide and develop into mature cells, acting as a maintenance system for the body. MSCs help to maintain homeostasis in the body through two primary functions: maintaining the number of adult cells at a constant level through duplication and replacing damaged cells through differentiation.
- Stem cells have a unique property that causes them to migrate toward inflammation, areas where they are needed for tissue repair. Here, the cells seed themselves into damaged tissue to mature into functional cells. Read more.
- MSCs also coordinate the healing process through a process call "signaling." Cell signaling is the body's way of communicating in real time to coordinate our innate repair system. Through this system of cellular communication, MSCs regulate the immune response by attracting cells to areas where they are most needed. Cell signaling takes place via the paracrine system to regulate the behavior of existing cells. Stem cells act as team captain, directing the healing response and monitoring the regenerative environment by regulating inflammation, remodeling, repair and cellular recruitment. Recently, 80% of the therapeutic effect of stem cells is attributed to their release of protein growth factors that signal cells to facilitate growth/repair.
- The repair process itself occurs with a process called "translation,” the actual formation of protein molecules. Stem cells are also a regulatory factor in a complex cellular process called "protein synthesis.” They release large amounts of proteins and growth factors (GF), nucleic acids, exosomes, and microRNA.
Understanding of the important role stem cells play in the healing process accentuates the need for examination of steroid use. In a 2014 blog by Chris Centeno, MD published by Regenexx, he discusses research regarding the detrimental use of corticosteroids. In particular, a 2015 study by Cody C. Wiles and colleagues examines cytotoxicity of corticosteroids on mesenchymal stem cells. The study by Wiles explains that “Exposure to corticosteroids decreased MSC viability in a curvilinear dose-response pattern.”
A Better Approach
So why does cortisone remain a standard practice for many physicians? The answer is simple. It is quick, easy, and works... for a short period of time. Long-term however, corticosteroid use causes more harm than good. Educating patients about how their body heals and how they can enhance the healing process not only helps patients make better choices, but also helps advance medical treatment.
Mayo Clinic, a leader in development of Regenerative Medicine, has recently developed a program dedicated to research training programs in regenerative sciences and how these discoveries translate into clinical medicine. Training at Mayo Clinic and studies by clinics across the country are helping to advance Regenerative Medicine as a standard treatment for multiple conditions, effectively changing the paradigms in healthcare.
Regenerative medicine offers a transformative approach to treating musculoskeletal conditions by harnessing the body's natural healing capabilities.
MSCs offer a potential regenerative solution given their ability to differentiate to all tissues within a joint and modulate the local inflammatory response. Although these characteristics suggest they provide ideal building blocks to restore damaged joints, a strong body of evidence supports MSC-guided regeneration through paracrine stimulation of native tissue. Wiles et al.
Research has shown definitively that the body can heal itself. Recently, scientists have recently discovered just how this works on a cellular level. From this knowledge, physicians have designed innovative procedures that harness the body's innate healing mechanisms to promote long-term recovery rather than temporary symptom relief.
While high-dose corticosteroid injections can provide short-term relief for musculoskeletal conditions, the potential for significant adverse effects makes them a less-than-ideal long-term solution. Regenerative medicine offers a promising alternative, focusing on natural healing and tissue repair. Explore safer and more effective options for managing musculoskeletal health.


