The field of regenerative medicine is complex. Patients often believe that the treatment they receive at one clinic is the same as another, that the latte at this Starbucks is the same as the latte at another. But all Regenerative Orthopedic procedures are not created equal. Patients often purchase a stem cell procedure using dead umbilical cord or amniotic cells or the bone marrow aspirate is not correctly processed. With subpar processing of Platelet Rich Plasma, the concentration is not sufficiently condensed. Or, often the procedure is performed by a low-level provider that is “overseen” by a medical doctor. As part of our patient awareness campaign, we are presenting what we feel are important criteria when selecting a who you trust for YOUR musculoskeletal treatment.
Who performs your procedure matters!

Board Certification is the standard in medical training. Several years of residency training followed by successful written and oral exams results in certification by a board in the respective medical specialty. These boards are, in turn, overseen by the American Board of Medical Specialties. Regenerative Medicine has no ABMS accepted board. Because Regenerative Medicine has no legitimate board certification, the skill levels are so different that it is startling.
Most patients believe that all physicians are trained the same and that a PRP or “stem cell” injection is the same wherever they go, just like a Starbucks Latte is the same. However, the vast difference in provider skill and injection training, along with patient misconception of parity in training, can have critical results. Knowledge of how to precisely place stem cells into the musculoskeletal system matters. While many clinics claim to be experts in the area of using stem cells to heal orthopedic injuries, they’re not. In fact, they’re in a place of not knowing what they don’t know.
Developing regenerative specialties in many medical schools will hopefully eliminate unqualified providers. For now, however, the patient needs to do their homework. Fortunately, Regenexx has done some of that homework for you by striving to standardize physician qualifications, procedures and use of processing kits.
Many clinics promote dubious procedures and questionable products. They use unqualified staff to perform the procedure. To bypass legal requirements, a physician, whether or not qualified in regenerative procedures, “oversees” the procedure. Provider qualification is the most crucial criteria when selecting a clinic providing Regenerative Orthopedics. Make certain you know who will be performing the procedure and their qualifications and knowledge.
Qualified regenerative orthopedic physicians have detailed knowledge of the musculoskeletal system. They understand how it functions and what can go wrong. Treatment by an unqualified provider with minimal training follows the textbook description of the procedure. This is not the best approach. When variations occur, they are unlikely to adapt to individual patients. The physician specialty trained in musculoskeletal conditions understands what to do, how to tailor the procedure to your individual condition and anatomy. An untrained provider, generally, does not have the knowledge or experience to make adjustments to inject into a more precise location. Watch out that you are getting what you think you are paying for!
Ask WHO will actually be performing the procedure and
what their qualifications are.
Dosage Matters!
To ensure the success of platelet-rich plasma (PRP) treatment, it is essential that the proper concentration and dose is given to patients to maximize a positive outcome. Chris Centeno, MD, an international expert in Interventional Orthopedics and Regenexx Founder, recently addressed how patients can recognize whether they are getting a high-quality PRP product that meets the criteria needed for a maximally successful outcome.
PRP is created by taking whole blood from the patient, usually from a vein in the arm, and then centrifuging it to concentrate the platelets in plasma. This solution contains healing growth factors and exosomes that support tissue healing. Four factors affect PRP quality:
- Body locations treated
- Use of imaging guidance
- Type of PRP
- Dose
A key benefit in the use of Regenexx regulated procedures is the compilation of data, extensive research, and consistency of procedure that result in credible information. Data regarding dosage is particularly beneficial in PRP success rates. Below, Dr. Centeno presents recommended dosages for patient knowledge when shopping for a regenerative facility.
PRP dose and age: For young patients, a lower platelet concentration (2-3x PRP) often contains sufficient growth factors for a positive response. However, middle-age and older patients have older cells that are generally poor in growth factors, requiring a more highly concentrated PRP solution. Table 1 below shows concentrations/doses by age that are typically effective.

The above table was created by Dr. Centeno’s observations of his clinic’s in-vitro data, his published work on young vs old tenocytes, and nearly two decades of clinical experience.
Although some patients respond to lower doses than listed in Table 1, most need the dosages similar to those shown to maximize their response. Notably, the amount of whole blood needed to get 10-20 ml of injectate PRP to reach the 14-20x level can be large (about the volume of a standard blood bag).
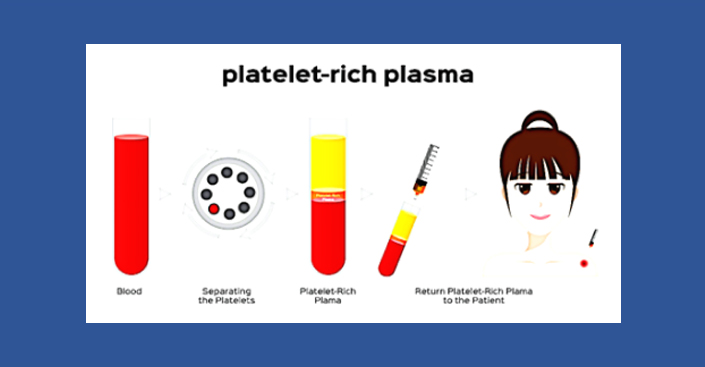
Because patients don’t generally know which PRP systems the provider clinic uses to create PRP for injection, it is difficult for patients to assess whether they are getting an effective injection. Table 2 shows the volumes needed to prepare a PRP injectate for maximum benefit.
Generally, a 3 mL injection of PRP is enough to inject a single large joint like a knee, hip, or shoulder. Volume varies depending on how many joints and size of joint(s). The efficiency of the platelet capture is never 100%. Bad systems are about 50% efficient at capturing platelets; good systems can be 80%.
Example case: Peggy, an older woman, wants to continue hiking and staying active, but her arthritic knee is making it painful. The physician determined that she would need 3 mL of 14-20x PRP injected into the knee joint. According to the table, she would need to have 80 mL of whole blood drawn to obtain 3 ml of 14-20x PRP for injection.
“If you’re older, pay attention to how much blood is being drawn and use the tables above to
determine whether you’re getting a high-quality PRP injection for your money!”
False Labeling and Untrue Claims!
Cellular therapies and their use in regenerative medicine hold almost infinite possibilities for curative treatments. Scientific advances in the understanding of how the body actually heals through tissue regeneration, combined with rapid developments in stem cell biology, have truly created a renaissance in medical treatment. However, Regenerative Medicine remains in its early stages and its use has grown with little regulation. Hundreds of clinics have opened around the country making unproven claims. With all the varying perspectives, information, and misinformation, combined with an influx of stem cell clinics, sorting out this large volume of information is difficult, even for medical professionals.
As this fascinating field continues to mature, a small number of clinics have attached a “stem cell” label to products and procedures that do not actually contain live stem cells. Using overstated or false claims enables disreputable clinics to easily exploit desperate patients. These unscrupulous clinics stand in the way of sincere efforts to discover and provide treatments for conditions that previously had few options.
Bone marrow transplants have been used for many years to treat blood diseases. Haematopoietic stem cells (HSCs), produced in the marrow are responsible for maintaining blood production throughout our lives, including cells needed for the immune system. Discovered in the 1960s, they are the first stem cells to be discovered.
Mesenchymal stem cells, MSCs, are the type of stem cells used in efforts to regenerate tissue in joints. Joint tissue traditionally heals slowly and incompletely due, primarily, to poor blood supply. Read more. Healing of musculoskeletal conditions requires that our bodies are able to supply the necessary healing units. “Dynamic Equilibrium” exists when cell degeneration is in equal ratio to cells available for regeneration. Injury, arthritis and poor cellular health disrupt this homeostasis. Adequate cells for repair are unable to keep pace with healing requirements.
Chronic injury generally results in uncontrolled inflammation as our body struggles to supply healing nutrients and growth factors. Our body senses injury and responds as it does with any injury: through cell signaling, rushing the necessary cells to the site. This process is miraculous and keeps our bodies healthy. When the injury does not heal completely, the process known as inflammation becomes uncontrolled, causing further damage to tissue and arthritis. Localized stem cells, critical in the process, become depleted. Read more.
Bone marrow stem cells (BMSCs) are the only stem cell-based products FDA approved for use in the US, meeting standards of minimal manipulation and homologous use. Cells areharvested from the patient’s hip, minimally processed on site and injected into the site of injury. These viable stem cells differentiate into cells of target tissue and integrate into this tissue, regenerating tissue to replace necrotic, or damaged, cells. Physicians may use a booster of Platelet Rich Plasma, PRP, in the solution itself to provide growth factors and nutrients helpful in the healing process.
Labeling of amniotic tissue as “stem cell therapy” is a primary concern in Regenerative Orthopedics for physicians trained and certified in cellular biologic use of stem cells. The FDA has established the criteria shown below for the use of stem cells in the US.
The FDA is currently addressing several key issues to ensure legitimate medical use:
- Claims of effectiveness
- Viability of source and processing methods
- Clinical studies to ensure effectiveness
- Qualification of professionals performing the procedure
Chris Centeno, MD discusses the use of non-viable cells presented to patients as living stem cells in a 2017 blog. Unfortunately, the problem is still relevant. Centeno blog 2017
Christopher J. Centeno, MD, is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine.
Do your homework. Know the qualifications of the rendering provider and the quality of processing system the provider is using. We want you to be informed in the best possible way of the most important elements when making this decision.
****

As a professional, I strive to learn the safest and most effective treatments available. My continued commitment and training to advance this field of medicine separates me from the many disreputable “Stem Cell” clinics with their false labeling and false claims of effectiveness that have been popping up throughout the country. Qualifications of physicians in these clinics with their unproven claims is a primary concern for physicians trained and certified in cellular biological use of stem cells. I welcome FDA oversight to keep this fledgling field of medicine on the right track.
I believe that health care is no longer merely the treatment of disease. We all want to live longer, live better and live healthier. We no longer want medications that treat pain but mask injury, procedures that cut and sew. I have helped thousands of patients find freedom from pain to restore their quality of life. I want to help you!
Who is doing your procedure?
